The modern diet contains a large number of simple sugars. From bread to donuts, to carbonated drinks to chocolate, cookies, and candy, everywhere you look, temptation abounds. The potential impact on the health of diets rich in free sugars, and particularly fructose, is of major concern. Does the sugar we take have an impact on insulin resistance and obesity? In this article, we look at this risk and the effects of insulin resistance.
- Sugar and Insulin resistance….
Sugar has a bittersweet reputation when it comes to health. It occurs naturally in all foods that contain carbohydrates, such as fruits and vegetables, grains, and dairy. Consuming whole foods that contain natural sugar is safe. Plant foods also have high amounts of fiber, essential minerals, and antioxidants, and dairy foods contain protein and calcium.
Where does the problem with sugar come about? Added sugar, which is usually extracted or synthesized ……
There is plenty of evidence to suggest that consuming too much sugar can have a negative effect on our metabolic health. Regular sugar consumption produces a constant release of the hormone insulin. Over a period of time, it can lead to serious problems, such as the synthesis of triglycerides, insulin resistance, fatty liver disease, type II diabetes, an increase in very-low-density lipoprotein (the bad kind of cholesterol), and the accumulation of fat on all tissues.
Added sugar intake may contribute to and certainly does exacerbate insulin resistance. For example, added sugar intake is associated with higher blood pressure, inflammation, weight gain, fatty liver disease, health issues that can lead to insulin resistance, and further exacerbation of these issues. Added sugars cater to particularly energy-hungry but metabolically inefficient cells, including senescent cells, cancerous cells, and even quickly proliferating pathogenic bacteria in the gut.
Several genetic and lifestyle factors can contribute to how likely you are to develop insulin resistance. But even if you have a genetic risk, you can help yourself with regular exercise, a balanced diet, avoidance of added dietary sugars, healthy sleep patterns, and stress reduction activities.
Risk factors for insulin resistance and prediabetes include:
- Obesity
- Aging
- physical inactivity
- high cholesterol
- blood pressure
- sleep disorders or circadian rhythm disruption
It is said that one in three Americans—including half of those age 60 and older— have insulin resistance.
- What exactly is Insulin Resistance?
Insulin resistance is when cells in your muscles, body fat, and liver start resisting or ignoring the signal that the hormone insulin is trying to send out—which is to grab glucose out of the bloodstream and put it into our cells. Glucose, also known as blood sugar, is the body’s main source of fuel. We get glucose from grains, fruit, vegetables, dairy products, and drinks that bring break down into carbohydrates.
- How does Insulin Resistance develop?
While genetics, aging, and ethnicity play roles in developing insulin sensitivity, the driving forces behind insulin resistance include excess body weight, too much belly fat, a lack of exercise, smoking, and even not getting enough sleep.
As insulin resistance develops, your body fights back by producing more insulin. Over months and years, the beta cells in your pancreas have been working so hard to make insulin get worn out and can no longer keep pace with the demand for more and more insulin. Then – years after insulin resistance silently began – your blood sugar may begin to rise, and you may develop prediabetes or type 2 diabetes. You may also develop non-alcoholic fatty liver disease (NAFLD), a growing problem associated with insulin resistance that boosts your risk for liver damage and heart disease.
- What are the Signs and Symptoms of Insulin Resistance?
Insulin resistance can be triggered by a combination of factors linked to weight, age, genetics, being sedentary, and smoking.
– Polycystic ovary syndrome (PCOS): Insulin resistance can worsen the symptoms of PCOS, which can include irregular menstrual cycles, infertility, and periods that cause pain.
– A large waist. Experts say the best way to tell whether you’re at risk for insulin resistance involves a tape measure and a moment of truth in front of the bathroom mirror. A waist that measures 35 inches or more for women and 40 or more for men (31.5 inches for women and 35.5 inches for men if you’re of Southeast Asian, Chinese, or Japanese descent) increases the odds of insulin resistance and metabolic syndrome, which is also linked to insulin resistance.
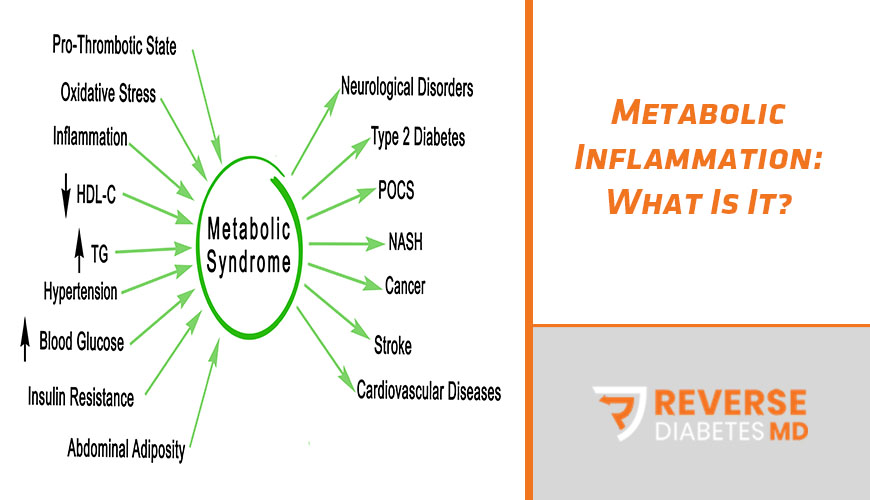
– You have additional signs of metabolic syndrome. According to the National Institutes of Health, in addition to a large waist, if you have three or more of the following, you likely have metabolic syndrome, which creates insulin resistance.
- High triglycerides. Levels of 150 or higher, or taking medication to treat high levels of these blood fats.
- Low HDLs. Low-density lipoprotein levels below 50 for women and 40 for men – or taking medication to raise low high-density lipoprotein (HDL) levels.
- High blood pressure. Readings of 130/85 mmHg or higher or taking medication to control high blood pressure
- High blood sugar. Levels of 100-125 mg/dl (the prediabetes range) or over 125 (diabetes).
- High fasting blood sugar (or you’re on medicine to treat high blood sugar). Mildly high blood sugar may be an early sign of diabetes.
– Acanthosis nigricans: This skin condition can develop in people with insulin resistance. It involves dark patches forming on the groin, armpits, and the back of the neck.
- What health conditions are related to Insulin Resistance?
The most common health condition related to Insulin Resistance is prediabetes and the resultant Type 2 Diabetes. Insulin resistance also doubles your risk for heart attack and stroke – and triples the odds that your heart attack or ‘brain attack’ will be deadly.
Insulin resistance and metabolic syndrome are also linked with a higher risk for cancers of the bladder, breast, colon, cervix, pancreas, prostate, and uterus. This is because the high insulin levels early in insulin resistance seem to fuel the growth of tumors and suppress the body’s ability to protect itself by killing off malignant cells.
Furthermore, research has found a strong association between insulin resistance and memory function decline, increasing the risk of Alzheimer’s disease.
- Can you prevent or reverse insulin resistance?
The good news is that, yes, insulin resistance can be prevented and also reversed in some cases. Here is what you can do:
- Get recommended amounts of physical activity and structured exercise
- Get adequate sleep
- eat when the sun is up(we are more insulin resistant at night and after a night of poor sleep, due to disrupted circadian rhythms that help regulate our metabolic state)
- Reducing stress and, therefore stress-related inflammation
- Maintaining a healthy weight
- Increasing your plant fiber intake.
All of the above can help improve your insulin sensitivity. It has been shown that combining both diet and exercise have the most impact on insulin sensitivity.
In a fascinating University of New Mexico School of Medicine, study published in the International Journal of Obesity, overweight people who lost 10% of their weight through diet plus exercise saw insulin sensitivity improve by an impressive 80%. Those who lost the same amount of weight through diet alone got a 38% increase. And those who simply got more exercise, but didn’t lose much weight, saw almost no shift in their level of insulin resistance.
Intermittent fasting is also another way in which you can reverse your insulin resistance. This is because it gives your body a break from insulin and glucose signaling pathways that promote cell proliferation and inflammation and may help increase insulin sensitivity.
- What, therefore, is the relationship between sugar and Insulin Resistance?
There is an association between diets high in sugars (predominantly sucrose) and the risk of disease, and experimental studies have shown that high intakes of fructose (over 100 g/d) can reduce insulin sensitivity. However, somewhat lower intakes may affect serum TG. The mechanisms for such associations or effects have not been convincingly demonstrated.
References:
- NCBI (2016): A review of recent evidence relating to sugars, insulin resistance, and diabetes. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5174139/
- Endocrineweb (2019): Insulin resistance causes and symptoms. Retrieved from https://www.endocrineweb.com/conditions/type-2-diabetes/insulin-resistance-causes-symptoms
- Medical News Today (2019): What to know about insulin resistance. Retrieved from https://www.medicalnewstoday.com/articles/305567.php
- The Sugar Movement (2016): Sugar vs Fat. Retrieved from https://thatsugarmovement.com/sugar-vs-fat/
- Harvard Health Publishing (2017): The sweet danger of sugar. Retrieved from https://www.health.harvard.edu/heart-health/the-sweet-danger-of-sugar
- NCBI (2014): Weight Loss, Exercise, or Both and Cardiometabolic Risk Factors in Obese Older Adults: Results of a Randomized Controlled Trial https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3835728/