The very mention of a ketogenic diet can throw some physicians into a tailspin. As physicians, we are taught about diabetic ketoacidosis, a potentially life-threatening medical emergency. We are not routinely taught about nutritional ketosis, the default human state of existence.
Our brain requires either glucose or ketones as a primary fuel source. Ketones are a vital evolutionary advantage, since we have only about 24 hours storage capacity for glucose or glycogen (500g total), but a nearly unlimited supply of ketones converted from fat. As a species we would have all died out, but for the ability to survive in nutritional ketosis.
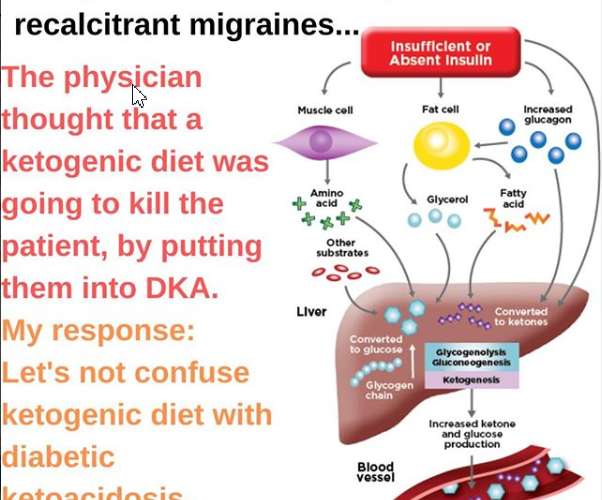
Diabetic ketoacidosis occurs when diabetics with no insulin production (usually Type I diabetics, or late-stage insulin-dependent Type II) enter cellular starvation despite high circulating glucose. Without insulin, they can’t get glucose into their cells and start to have organ failure with a drop in pH. They then enter into starvation recovery mode and generate ketones out of fat and proteins. By the time ketone levels approach 15 to 25 mm, the resulting pH imbalance leads to profound metabolic derangement.
Nutritional ketosis does not have a metabolic derangement, because the feedback loop of insulin clears the bloodstream of excessive circulating glucose, and the ketones being produced are used for energy or exhaled. Nutritional ketosis maintains beta-hydroxybutyrate levels between about 0.5 and 3.0 mM, far less than the levels required to cause acid-base abnormalities. Longterm, keto-adaption the brain shifts from being primarily dependent on glucose, to being primarily dependent on beta-hydroxybutyrate.