Reverse Diabetes MD Presentation | Reverse Diabetes MD from Gurpreet Padda on Vimeo.
It’s time to take a more detailed look at the root causes of obesity, prediabetes, and type 2 diabetes because of the implication for future public health. Reversing the obesity, prediabetes, and type 2 diabetes epidemic is today’s most important public health challenge. Nearly 70% of population is insulin resistant, prediabetic, or frankly diabetic.
Kraft, J.R.:” Glucose Insulin Tolerance. A routine Clinical Laboratory Tool Enhancing Diabetes Detection”. In O.B. Hunter. Jr. (ed): Radio assay: Clinical Concepts. Skokie, IL. Professional Education Dept. G.D. Searie& Co., 1974. Pp 91-106
Using data from the National Health and Nutrition Examination Survey 2009-2016, less than 12.2% of the US population is now considered metabolically healthy.
“Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009-2016,” was published online Nov. 28 in the journal Metabolic Syndrome and Related Disorders.
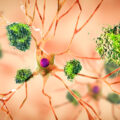
Almost all the patients who present to our clinics are overweight, and when we evaluate their biochemical markers, they have prediabetes and metabolic inflammation. Pre-diabetes is known to be a condition that precedes type 2 diabetes (T2D). The changes in immune cells concentration and function can cause an increased migration of these inflammatory cells to already inflammed tissue. There is also upregulation of cytokines. This immune activation begins during the pre-diabetic state.
According to studies published in a cardiovascular and heart disease prevention journal in Europe, “The increased risk of adverse cardiovascular outcomes associated with type 2 diabetes does not begin at the diagnostic cutoff for plasma glucose (or HbA1c) at which the condition is diagnosed. Rather, there appears to be a continuum of increased microvascular and macrovascular risk that extends to levels of glycemia well below these cutoffs.”
Hopper I, Billah B, Skiba M, Krum H. Prevention of diabetes and reduction in major cardiovascular events in studies of subjects with prediabetes: meta-analysis of randomized controlled clinical trials. Eur J Cardiovasc Prev Rehabil. 2011;18:813–823. [PubMed]
A 2015 global survey carried out by Credit Suisse revealed a substantial level of misinformation that exists among doctors and nutritionists:
- 92% believed that fat consumption could lead to cardiovascular issues
- 87% believed that fat consumption could lead to obesity
- 54% of doctors and 40% of nutritionists thought that eating cholesterol-rich foods raised blood cholesterol
- 83% of doctors believed butter was worse than margarine
- 66% of doctors believed vegetable oils are beneficial to health.
Fat; The New Health Paradigm – Credit Suisse 2015
The fact that prescription medications are now the third most common cause of death globally after heart disease and cancer should be alarming. The Academy of Medical Royal Colleges and the BMJ provide a blueprint to reduce the harms of “too much medicine” as part of the Choosing Wisely campaign, with recommendations to educate the public to ask their medical professionals whether there are “simpler or safer options” to taking a medication.
Malhotra A, Maughan D, Ansell J, Lehman R, Henderson A, Gray M et al. Choosing Wisely in the UK: The Academy of Medical Royal Colleges’ initiative to reduce the harms of too much medicine BMJ 2015; 350 :h2308.
The root cause of obesity, prediabetes, and type 2 diabetes are embedded in the food environment. Legislative efforts to encourage less consumption of processed foods and sugary drinks will help significantly reduce the burden of diet-related disease, which now contributes to more disease and death globally than physical inactivity, smoking and alcohol combined.
Newton JN, Briggs AD, Murray CJ, Dicker D, Foreman KJ, Wang H, et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015. doi:10.1016/S0140-6736(15)00195-6.
Processed foods labelled as “low-fat” or “proven to lower cholesterol” should be avoided. The flawed science behind the 1977 Dietary Guidelines promoted a reduction in fat consumption, which permitted an increase in carbohydrate consumption. The shift from natural food containing animal products and fats resulted in an increase in processed food consumption rich in carbohydrates, processed grains, and industrial seed oils. In the United States between 1961-2011, 90% of the increased calorie intake has come from carbohydrates and polyunsaturated vegetable oils.
Select Committee on Nutrition and Human Needs. Dietary goals for the United States. First ed. Washington: U.S. Govt. Print. Off., February 1977.
CreditSuisse.Fat: The New Health Paradigm: Research Institute, 2015: 76
The rise in obesity following these guidelines suggest that they may be a root cause of the problem. Nutrition science was originally founded on human correlational studies, which are frequently flawed. But that science has also been corrupted by commercial influences. The undue influence of the food industry on official guideline bodies and politicians has posed a significant threat to public health. “Nutritional epidemiology is a scandal. It should just go to the waste bin,” claims professor John Ioannidis, professor of medicine, health research and policy, and statistics at Stanford University School of Medicine and School of Humanities and Sciences.
Max Planck also said, “Science progresses one funeral at a time.” it took nearly 50 years from the first published scientific evidence linking smoking and lung cancer until effective regulation was introduced to curb tobacco consumption. Big tobacco companies adopted a strategy of denial, planting doubt, obfuscating, and even buying the loyalty of scientists. The recent similarities with big food and big pharma are uncanny.
Brownell KD, Warner KE. The perils of ignoring history: big tobacco played dirty and millions died. How similar is big food? Milbank Q 2009;87: 259–94.
The food industry has a fiduciary responsibility to produce profit for their shareholders. Unfortunately, the food industries’ downstream cost to public health is bankrupting most westernized societies. Unfortunately, academics, institutions and journals whose primary responsibility is to patients and scientific integrity have at times colluded with industry for financial gain. It is incredulous to suggest that consuming 22 teaspoons of sugar daily falls within recommended guidelines. This is despite the known science that for optimum health there is no dietary or biological requirement for sugar to be consumed in the human diet.
Malhotra, A. (2013) The dietary advice on added sugar needs emergency surgery. BMJ, 346, f3199.
Evidence from multiple randomized controlled trials reveals that a higher-fat, lower-carbohydrate diet is superior to a low-fat diet for weight loss and cardiovascular disease risk reduction. A meta-analysis of 53 randomized controlled trials involving 68,128 participants conducted by the Harvard School of Public Health concluded that “when compared with dietary interventions of similar intensity, evidence from randomized controlled trials does not support low-fat diets over other dietary interventions for long-term weight loss. In weight loss trials, higher-fat weight loss interventions led to significantly greater weight loss than low-fat interventions.”
Sackner-Bernstein J, Kanter D, Kaul S. Dietary Intervention for Overweight and Obese Adults: Comparison of Low-Carbohydrate and Low-Fat Diets. A Meta-Analysis. PLoS One 2015;10(10):e0139817 DOI: 10.1371/journal.pone.0139817[published Online First: Epub Date]|.
Bazzano LA, Hu T, Reynolds K, et al. Effects of Low-Carbohydrate and Low-Fat Diets: A Randomized Trial Effects of Low-Carbohydrate and Low-Fat Diets. Ann. Intern. Med. 2014;161(5):309-18 DOI: 10.7326/M14-0180[published Online First: Epub Date]|.
Harcombe Z, Baker JS, Cooper SM, et al. Evidence from randomized controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart 2015;2(1) DOI: 10.1136/openhrt-2014-000196[published Online First: Epub Date]|.
The Women’s Health Initiative, one of the largest randomized controlled diet trials ever performed, used 48,835 post-menopausal women, with a mean follow-up period of 8.1 years, randomized to either a standard western diet or a low-fat, calorie-reduced diet with increased exercise. The authors had postulated that a low-fat, calorie-reduced diet with increased exercise would reduce cardiovascular disease. The intervention achieved an 8.2% energy decrease in total fat intake and a 2.9% energy decrease in the saturated fat intake but did not reduce risk of CHD or stroke. The reduction in dietary fat and total daily calories (361 calories/day reduction) failed to produce any significant weight loss over the duration of the study, thus rejecting the hypothesis that the low-fat diet is either beneficial for cardiovascular disease or weight loss.
Howard BV, Van Horn L, Hsia J, et al. Low-fat dietary pattern and risk of cardiovascular disease: The Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295(6):655-66 doi: 10.1001/jama.295.6.655[published Online First: Epub Date]|.
By contrast, consumption of fat induces satiation and when compared to the other macronutrients such as protein and carbohydrates, fat has the least impact on blood glucose and insulin production. Excessive insulin production and subsequent insulin resistance is the precursor to type 2 diabetes. A meta-analysis of the evidence available prior to the 1977 US change in dietary guidelines did not support the dietary fat restrictions. Despite the lack of scientific consensus, these guidelines advised to limit total fat to 30% of calorie intake and saturated fat to 10% of calorie intake, creating the low-fat craze and a national experiment on diet-induced metabolic dysfunction.
Harcombe Z, Baker JS, Cooper SM, et al. Evidence from randomized controlled trials did not support the introduction of dietary fat guidelines in 1977 and 1983: a systematic review and meta-analysis. Open Heart 2015;2(1) doi: 10.1136/openhrt-2014-000196[published Online First: Epub Date]|.
Thirty years later, in 2014, a meta-analysis of 76 studies with over 600,000 participants from 18 countries concluded that “Current evidence does not clearly support cardiovascular guidelines that encourage high consumption of polyunsaturated fatty acids and low consumption of total saturated fats.”
Chowdhury R, Warnakula S, Kunutsor S, et al. Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2014;160(6):398-406 doi: 10.7326/M13-1788[published Online First: Epub Date]|.
A study published in the BMJ (British Medical Journal) noted that “Saturated fat intake was not associated with all- cause mortality, CVD mortality, total CHD, ischemic stroke, or type 2 diabetes.”
de Souza RJ, Mente A, Maroleanu A, et al. Intake of saturated and trans unsaturated fatty acids and risk of all-cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ 2015;351 doi: 10.1136/bmj.h3978[published Online First: Epub Date]|.
Further, The American Journal of Clinical Nutrition found that “diets with cheese and meat as primary sources of saturated fatty acids cause higher HDL cholesterol and apo A-1 and, therefore, appear to be less atherogenic than is a low-fat, high- carbohydrate diet.”
Thorning TK, Raziani F, Bendsen NT, Astrup A, Tholstrup T, Raben A. Diets with high-fat cheese, high-fat meat, or carbohydrate on cardiovascular risk markers in overweight postmenopausal women: a randomized crossover trial. The American journal of clinical nutrition 2015 doi: 10.3945/ajcn.115.109116[published Online First: Epub Date]|.
Full-fat dairy may protect against obesity. A 2014 study concluded: “Participants in the highest tertile of whole-fat dairy intakes (milk, cheese, yogurt) had significantly lower odds for being obese. “
Crichton GE, Alkerwi Aa. Whole-fat dairy food intake is inversely associated with obesity prevalence: findings from the Observation of Cardiovascular Risk Factors in Luxembourg study. Nutrition Research 2014;34(11):936-43 doi: 10.1016/j.nutres.2014.07.014[published Online First: Epub Date]|.
Cohort studies confirm that plasma saturated fatty acids from dairy sources such as cheese and yogurt are inversely related to the incidence of type 2 diabetes. By contrast, the plasma saturated fat palmitic acid, linked to the consumption of starch, sugar and alcohol, is strongly associated with the development of type 2 diabetes.
Mozaffarian D. Saturated fatty acids and type 2 diabetes: more evidence to re-invent dietary guidelines. Lancet Diabetes Endocrinol 2014;2:770–2
Natural, non-processed, non-refined food (meat, fish, eggs, nuts, seeds, olive, avocados) contains high levels of saturated fat. These natural foods are a portion of the ancestral human diet. People have eaten as much as they want to of these foods without adverse health consequences since paleolithic times, until 1977 when the Dietary guidelines demonized saturated fat of omnipresent natural fat, driving people away from highly nourishing, wholesome and health-promoting foods.
Reducing dietary saturated fats does not reduce cardiovascular events and death. Improvements in cardiovascular outcomes are independent of direct cholesterol lowering. Dietary trials that provide abundant natural fats such as α-linoleic acid, polyphenols and Ω-3 fatty acids found in nuts, olive oil, oily fish and vegetables exert a positive health effect, likely by reducing inflammation, atherosclerosis and thrombosis.
Chakrabarti S, Freedman JE. Review: nutriceuticals as antithrombotic agents. Cardiovasc Ther 2010;28:227–35.
Interestingly, replacing saturated fat with Ω-6 containing vegetable oils (highly processed and refined industrial seed oil) does lower LDL cholesterol but does not actually improve cardiovascular mortality, and may actually increase mortality.
Veerman J Lennert. Dietary fats: a new look at old data challenges established wisdom BMJ 2016; 353 :i1512
Total and LDL cholesterol are a poor marker of cardiovascular health. Cholesterol profile of elevated triglycerides and low HDL is a more predictive marker of cardiac risk and a reliable marker of insulin resistance. In fact, the QRISK calculator, used to estimate the 10-year risk of CVD, does NOT use LDL cholesterol, but uses total cholesterol/HDL ratio instead.
Preventing insulin resistance in young men would prevent 42% of myocardial infarctions, a larger reduction than correcting hypertension (36%), low high-density lipoprotein cholesterol (31%), body mass index (21%) or low-density lipoprotein cholesterol (16%).
Eddy D, Schlessinger L, Kahn R, Peskin B, Schiebinger R. Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Diabetes Care. 2009;32(2):361–6.
Refined Carbohydrates:
Prediabetes and Type 2 diabetes are diseases of insulin resistance with initial excessive insulin production, which display the symptom of elevated blood glucose levels as the disease progresses. Treating the root cause of the disease, instead of the symptom, is the key. Eliminate all refined carbohydrates to reverse obesity, prediabetes, and type 2 diabetes.
Refined carbohydrates are known to increase blood glucose levels, increase requirements for medications and result in weight gain. It is disturbing that dietary guidelines prioritize the consumption of starchy carbohydrates for type 2 diabetics, to nearly 55% of their daily macronutrient consumption. Such diets will potentially lead to progressive worsening of disease with all its attendant complications, such as blindness, kidney failure, nerve damage, peripheral vascular disease, heart disease and stroke.
Added sugar has no nutritional value whatsoever. There are no biochemical reactions in the human body that require dietary fructose. No single study exists that demonstrates benefit associated with its consumption.
Credit Suisse – Sugar Consumption at a crossroads
Dietary carbohydrate restriction is the “single most effective intervention for reducing all of the features of the metabolic syndrome” according to Credit Suisse, and should be the first approach in diabetes management. A ketogenic diet (one that comprises less than 10 percent of calorie intake from carbohydrates) results in the greatest falls in HbA1C and reduction in the use of medications. These benefits accrue independently of weight loss.
Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 2015;31:1–13.
Sugar+veg oil+grain=obesity®PreDM®T2D
Dietary sugar is strongly associated with increased risk of type 2 diabetes, hypertension, and cardiovascular disease, independent of its calories or its effects on body weight.
Lustig RH: Sickeningly sweet: does sugar cause type 2 diabetes? YES. Can J Diab (in press).
Isocaloric fructose restriction and metabolic improvement in children with obesity and metabolic syndrome. Lustig RH, Mulligan K, Noworolski SM, Tai VW, Wen MJ, Erkin-Cakmak A, Gugliucci A, Schwarz JM. Obesity (Silver Spring). 2016 Feb;24(2):453-60. doi: 10.1002/oby.21371. Epub 2015 Oct 26.
Added sugar intake and cardiovascular diseases mortality among US adults. Yang Q, Zhang Z, Gregg EW, Flanders WD, Merritt R, Hu FB. JAMA Intern Med. 2014 Apr;174(4):516-24. doi: 10.1001/jamainternmed.2013.13563.
Vegetable Oil:
Despite at least 2-3 million years of human history, only since 1917 have industrial seed oils been a significant part of the human diet, with a major uptick in consumption in the late 1970s. Linoleic acid (the Ω-6 fat in these vegetable oils) is extremely susceptible to oxidation, making foods rancid, but also oxidizing in the body. Linoleic acid, in non-processed whole food (seeds, nuts, fish, and eggs), coexists with vitamins, minerals, and antioxidants, protecting this highly susceptible polyunsaturated fat.
Free Radic Biol Med. 2001 Dec 1;31(11):1388-95. The stomach as a bioreactor: dietary lipid peroxidation in the gastric fluid and the effects of plant derived antioxidants. Kanner J, Lapidot T.
Curr Atheroscler Rep. 2009 Nov;11(6):403-10. Impact of circulating esterified eicosanoids and other oxylipins on endothelial function. Shearer GC, Newman JW.
A meta-analysis including almost 10,000 patients confirmed that high intake of Ω-6 oils (from vegetable oils/margarines) increases the risk of death and heart disease compared to saturated fat plus trans fat. Human research data suggest that we should remove these vegetable oils from our food supply for optimal health.
29.BMJ. 2013 Feb 4;346:e8707. doi: 10.1136/bmj.e8707. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. Ramsden CE1, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, Ringel A, Davis JM, Hibbeln JR.
Older data was confounded by the inclusion of Ω- 3 polyunsaturated fatty acid intake. This misrepresented the health benefits of Ω–6. Other studies, such as the Anti-Coronary Club trial, confirm that Ω–6 PUFA increases death and coronary heart disease compared to animal fat.
Christakis G, Rinzler SH, Archer M t al. Effect of the anti-coronary club program on coronary heart disease. Risk-factor status. JAMA 1966;198:597–604
The LA Veterans trial found that cancer mortality increases with the consumption of Ω–6 rich vegetable oils.
Pearce ML, Dayton S. Incidence of cancer in men on a diet high in polyunsaturated fat. Lancet 1971;1:464-7.
Animal studies have also found that Ω–6 PUFA promotes the growth of experimentally induced cancers, whereas Ω–3 inhibits their growth. Ω–6 rich vegetable oil ( such as sunflower and corn oil), is linked to the increased risk of death, coronary heart disease, and cancer in humans as well as the growth of cancer in animal models.
Am J Epidemiol. 1998 Feb 15;147(4):342-52. Adipose tissue Ω–3 and Ω–6 fatty acid content and breast cancer in the EURAMIC study. European Community Multicenter Study on Antioxidants, Myocardial Infarction, and Breast Cancer. Simonsen N1, van’t Veer P, Strain JJ, Martin- Moreno JM, Huttunen JK, Navajas JF, Martin BC, Thamm M, Kardinaal AF, Kok FJ, Kohlmeier L.
Cancer Res. 1988 Dec 1;48(23):6642-7. Effect of different levels of Ω–3 and Ω–6 fatty acids on azoxymethane-induced colon carcinogenesis in F344 rats. Reddy BS, Sugie S.
Why eat less, move more fails:
A calorie is a calorie only if it is incinerated in a bomb calorimeter, and the heat given off measured. Biologically derived calories from different foods have entirely different metabolic effects on the human body. Equal calorie portions of sugar, alcohol, meat or olive oil have widely differing effects on hormonal systems, including insulin and satiety signals such as cholecystokinin or peptide YY. It is irrelevant how many calories a portion of food on a plate contains. What matters is how our body responds to taking in and absorbing those calories, how they are metabolized, and the resulting level of satiety.
The current caloric reduction strategies promoted for weight loss are ineffective. Using the standard calorie reduction approach produces a probability of attaining a normal weight at 1 in 167, generating a greater than 99% failure rate.
Fildes A et al. Probability of an Obese Person Attaining Normal Body Weight: Cohort Study Using Electronic Health Records. Am J Public Health. 2015;105: e54–e59
It is wrongly assumed that excessive caloric intake is the root cause of obesity. A calorie of food energy has different metabolic fates depending upon the hormonal stimulation. That same calorie may be used to generate body heat or stored as body fat. Obesity is a disease of failed energy partitioning, not one of total energy intake. The primary driver of this partitioning is the hormone insulin. Insulin is specifically a fat storage growth hormone.
Focusing on calories in and calories out produces an inherent bias against high-fat food, which may be protective against obesity and related diseases. The simplistic calorie focus results in a dietary guideline supportive of starch and sugar replacement of fat, which promotes insulin resistance.
It is our hope that shifting focus away from calories and emphasizing a dietary pattern that focuses on food quality rather than quantity will reduce obesity, related diseases, and cardiovascular risk.
Malhotra A, DiNicolantonio JJ, Capewell S. It is time to stop counting calories, and time instead to promote dietary changes that substantially and rapidly reduce cardiovascular morbidity and mortality. Open Heart 2015;2(1) doi: 10.1136/openhrt-2015-000273[published Online First: Epub Date]|.
Yo-yo dieting with rapid weight loss and regain from fad dieting is detrimental to health. Such ‘weight cycling’ contributes to hypertension, insulin resistance and dyslipidemia, resulting in increased mortality risk and worse cardiovascular outcomes.
Mann T, Tomiyama AJ, Westling E, et al. Medicare’s search for effective obesity treatments: diets are not the answer. Am Psychol 2007;62:220–33.
LC + exercise ¹ health
In the Action for Health in Diabetes trial, no cardiovascular benefits were found on a low-calorie diet combined with increased physical activity in type 2 diabetic patients.
(Despite the significant weight loss even up to the maximum follow-up of 13.5 years, no health benefits could be found. )
Wing RR, Bolin P, Brancati FL, et al. Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. NEngl J Med 2013;369:145–54.
Exercise is not the solution:
It is widely accepted amongst the public and media that consuming more calories than we burn is the cause of the obesity epidemic, and therefore the solution is to just do more exercise.
Food and beverage companies have pushed this physical activity message to exonerate themselves. The very companies promoting processed and highly refined foods linked to the obesity epidemic have sponsored major sporting events. This association of ultra-processed food and soft drinks with sport is troubling. Celebrity endorsements give the wrong message, particularly to children.
Regular physical activity does have beneficial health effects, but weight loss is not one of them. In fact, there has been little change in our levels of physical activity in the past three decades, while the levels of obesity have increased.
Luke A, Cooper RS. Physical activity does not influence obesity risk: time to clarify the public health message. Int J Epidemiol 2013;42:1831–6.
It is time to bust the myth of physical inactivity and obesity: you cannot outrun a bad diet . A Malhotra, T Noakes, S Phinney Br J Sports Med bjsports- 2015-094911Published Online First: 22 April 2015 doi:10.1136/bjsports-2015- 094911
The time spent not eating, is more important than the time spent eating. Snacking will make you fat. It’s the chronic high insulin from the constant feeding.
There have been two major changes in our dietary habits since the 1970s, prior to the onset of the obesity epidemic. The change to a high-carbohydrate, low-fat diet has been well documented and has played an important role in causing obesity. However, the increase in meal frequency plays an equal if not larger role and has been largely ignored. In the 1970s, the average number of eating opportunities was three – breakfast, lunch and dinner. By 2005, that number had almost doubled. Now we eat breakfast, snack, lunch, snack, dinner and snack — and more often than not, each of these contains refined carbohydrates.
Cameron JD. 6 meals per day does not result in greater weight loss. Br J Nutr. 2010 Apr;103(8):1098-101
Popkin BM. Does hunger and satiety drive eating anymore? Am J Clin Nutr 2010;91:1342–7
Eating nearly continuously from the moment we arise to the moment we go to sleep becomes an opportunity to store food energy without a chance to burn it. Eating six times a day does not result in weight loss but tends to increase overall consumption of food. Snacks are produced for convenience and shelf stability and are filled with refined carbohydrates and often supplemented with Ω–6 vegetable oil. The hyper-processing of food contributes to a high glycemic index, and the grazing pattern of behavior results in a chronically elevated level of insulin, the fat storage hormone.
Reducing the frequency of our meals and eliminating snacking are simple ideas that were practiced widely before the obesity epidemic.
Additional references for RCT’s comparing low carb and low fat for weight loss
- Shai I, et al. Weight loss with a low-carbohydrate, mediterranean, or low-fat diet. N Engl J Med 2008;359(3);229–41.
- Gardner CD, et al. Comparison of the Atkins, Zone, Ornish, and learn Diets for Change in Weight and Related Risk Factors Among Overweight Premenopausal Women. The A to Z Weight Loss Study: A Randomized Trial. JAMA. 2007;297:969–977.
- Brehm BJ, et al. A Randomized Trial Comparing a Very Low Carbohydrate Diet and a Calorie-Restricted Low Fat Diet on Body Weight and Cardiovascular Risk Factors in Healthy Women. J Clin Endocrinol Metab 2003;88:1617–1623.
- Samaha FF, et al. A Low-Carbohydrate as Compared with a Low-Fat Diet in Severe Obesity. N Engl J Med 2003;348:2074–81.
- Sondike SB, et al. Effects of a low-carbohydrate diet on weight loss and cardiovascular risk factor in overweight adolescents. J Pediatr. 2003 Mar;142(3):253–8.
- Aude YW, et al. The National Cholesterol Education Program Diet vs a Diet Lower in Carbohydrates and Higher in Protein and Monounsaturated Fat. A Randomized Trial. Arch Intern Med. 2004;164:2141–2146.
- Volek JS, et al. Comparison of energy-restricted very low-carbohydrate and low-fat diets on weight loss and body composition in overweight men and women. Nutrition & Metabolism 2004, 1:13.
- Yancy WS Jr, et al. A Low-Carbohydrate, Ketogenic Diet versus a Low-Fat Diet To Treat Obesity and Hyperlipidemia. A Randomized, Controlled Trial. Ann Intern Med. 2004;140:769–777.
- Nichols-Richardsson SM, et al. Perceived Hunger Is Lower and Weight Loss Is Greater in Overweight Premenopausal Women Consuming a Low-Carbohydrate/High- Protein vs High-Carbohydrate/Low-Fat Diet. J Am Diet Assoc. 2005;105:1433–1437.
- Krebs NF, et al. Efficacy and Safety of a High Protein, Low Carbohydrate Diet for Weight Loss in Severely Obese Adolescents. J Pediatr 2010;157:252-8.
- Summer SS, et al. Adiponectin Changes in Relation to the Macronutrient Composition of a Weight-Loss Diet. Obesity (Silver Spring). 2011 Mar 31. [Epub ahead of print]
- Daly ME, et al. Short-term effects of severe dietary carbohydrate-restriction advice in Type 2 diabetes–a randomized controlled trial. Diabet Med. 2006 Jan;23(1):15–20.
- Westman EC, et al. The effect of a low-carbohydrate, ketogenic diet versus a low- glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr. Metab (Lond.)2008 Dec 19;5:36.
- Halyburton AK, et al. Low- and high-carbohydrate weight-loss diets have similar effects on mood but not cognitive performance. Am J Clin Nutr 2007;86:580–7.
- Dyson PA, et al. A low-carbohydrate diet is more effective in reducing body weight than healthy eating in both diabetic and non-diabetic subjects. Diabet Med. 2007 Dec;24(12): 1430-5.
- Keogh JB, et al. Effects of weight loss from a very-low-carbohydrate diet on endothelial function and markers of cardiovascular disease risk in subjects with abdominal obesity. Am J Clin Nutr 2008;87:567–76.
- Volek JS, et al. Carbohydrate Restriction has a More Favorable Impact on the Metabolic Syndrome than a Low Fat Diet. Lipids 2009;44:297–309.
- Partsalaki I, et al. Metabolic impact of a ketogenic diet compared to a hypocaloric diet in obese children and adolescents. J Pediatr Endocrinol Metab. 2012;25(7-8):697-704.